Your body does incredible things during pregnancy, and your metabolism is no exception. From the moment of conception, your Basal Metabolic Rate begins shifting to support new life, and those changes continue well into the postpartum period. Understanding how your BMR changes can help you make better nutrition choices during this important time. While our BMR calculator gives you a baseline number, pregnancy and postpartum create unique metabolic shifts that standard formulas do not fully capture. Important: Always follow your OB-GYN or midwife's specific nutrition guidance.
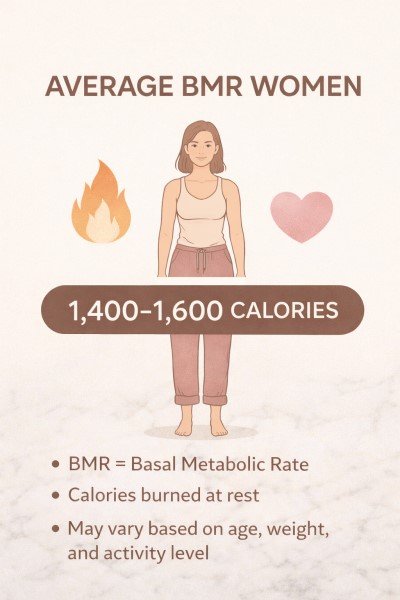
Whether you are currently pregnant, planning a pregnancy, or navigating the postpartum period, knowing what is happening with your metabolism can ease a lot of anxiety around food and weight. This guide breaks down the science in plain language so you can feel informed and empowered. For general context on female metabolism, you may also find our article on average BMR for women helpful as a starting reference point.
How Pregnancy Changes Your BMR
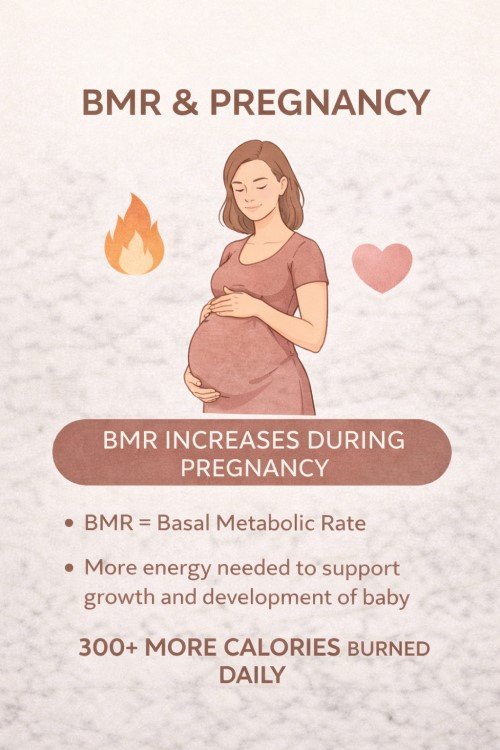
Pregnancy is one of the most metabolically demanding events the human body can experience. Your BMR rises gradually across all three trimesters to meet the growing energy demands of supporting a developing baby. In the first trimester, the increase is modest, around 5 percent, and most women do not need any extra calories during this stage. By the second trimester, BMR rises by roughly 10 percent, and guidelines suggest about 340 extra calories per day. In the third trimester, when metabolic demand peaks, BMR can increase by 20 to 30 percent, with an additional 450 calories per day recommended.
Why does your body need so much more energy? The reasons go far beyond the baby itself. Your body is building and maintaining a placenta, dramatically increasing blood volume, producing amniotic fluid, expanding breast tissue in preparation for nursing, and ramping up heart and lung function. All of these processes require fuel, and your elevated BMR reflects that increased demand.
| Trimester | BMR Change | Extra Calories* | Key Changes |
|---|---|---|---|
| First (weeks 1-12) | +5% | 0 extra | Morning sickness may limit intake |
| Second (weeks 13-26) | +10% | ~340/day | Baby grows rapidly |
| Third (weeks 27-40) | +20-30% | ~450/day | Maximum metabolic demand |
*Based on ACOG guidelines. Individual needs vary. Ask your doctor.
Not sure which trimester you're in? Use our pregnancy due date calculator to find your estimated due date and see your current week of pregnancy.
Why "Eating for Two" Is a Myth
One of the most persistent myths about pregnancy is that you need to eat double the amount of food. In reality, you do not need anywhere close to double the calories. As the table above shows, extra calorie needs are relatively modest, especially in the first trimester when many women need no additional calories at all. Overeating during pregnancy can lead to excessive weight gain, gestational diabetes, and complications during delivery.
What matters far more than quantity is quality. During pregnancy, your body has heightened needs for specific nutrients. Focus on nutrient-dense foods rich in folate, iron, calcium, protein, and omega-3 fatty acids. Leafy greens, lean meats, eggs, legumes, dairy or fortified alternatives, fatty fish (low mercury), and whole grains are all excellent choices. Prenatal vitamins are important, but they complement healthy eating rather than replace it. They fill in nutritional gaps but cannot substitute for a balanced, whole-foods diet.
For evidence-based guidance on pregnancy nutrition, the American College of Obstetricians and Gynecologists provides a thorough resource on nutrition during pregnancy.
BMR After Delivery: What to Expect
After giving birth, your BMR does not immediately snap back to pre-pregnancy levels. In the early postpartum weeks, your metabolism remains elevated as your body heals from delivery and, if you are breastfeeding, produces milk. Breastfeeding alone can burn an additional 300 to 500 calories per day, which is why many nursing mothers feel ravenously hungry and why adequate calorie intake during this time is so important.
For most women, BMR begins its gradual return to pre-pregnancy levels within a few months postpartum. However, full metabolic normalization can take six to twelve months or even longer. Several factors influence this timeline, including hormonal shifts (especially thyroid function), sleep deprivation, activity level, and whether you are nursing. Sleep deprivation in particular has a powerful effect on metabolism, disrupting hunger hormones like ghrelin and leptin and making it harder for your body to regulate energy efficiently.
The most important thing to remember is this: do not rush the process. Your body just did something extraordinary. Give it the time and nourishment it needs to recover properly.
Safe Postpartum Nutrition (Not Dieting)
The postpartum period is not the time for restrictive dieting. Most doctors recommend waiting at least six weeks after delivery before any intentional calorie restriction, and longer if you are breastfeeding. Cutting calories too aggressively while nursing can reduce your milk supply and leave you depleted of the nutrients you need for recovery.
Instead of dieting, focus on nourishing your body with the foods it needs most during this demanding time. Prioritize protein for tissue repair and recovery, as your body is healing from either vaginal delivery or a cesarean section. Stay well hydrated, especially if breastfeeding, as milk production requires significant fluid intake. Our water intake calculator can help you estimate your daily hydration needs. Include iron-rich foods to replenish stores that may have been depleted during pregnancy and delivery, and eat plenty of fiber to support digestive health, which can be sluggish postpartum.
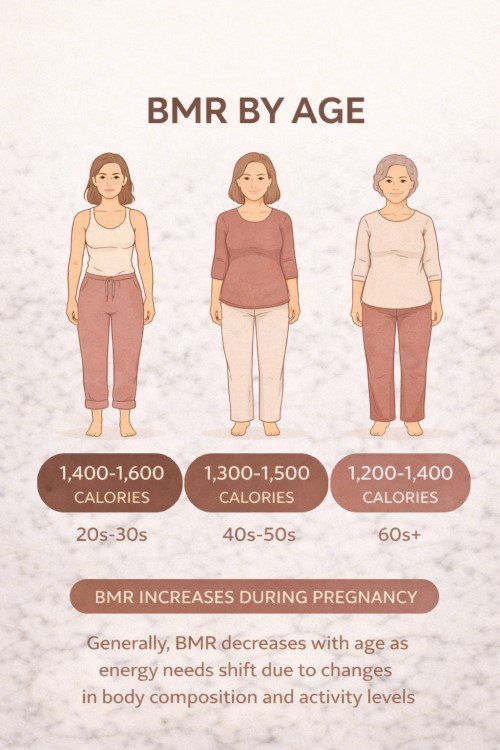
When your doctor clears you for gentle movement, start slowly with walks and light activity. There is no rush to return to intense exercise. For context on how your metabolic needs shift across life stages, see our guide on BMR by age for women.
When Can You Start Thinking About Weight Loss?
The earliest most women should consider intentional weight loss is after their six-week postpartum checkup, and many doctors recommend waiting even longer, particularly if you are breastfeeding. When you do begin, the approach should be gentle, gradual, and sustainable. Start with calorie awareness rather than strict deficits. Use our BMR calculator to find your current baseline, then factor in your activity level and breastfeeding status to determine an appropriate calorie target.
You may also find it helpful to check our BMI calculator and ideal weight calculator for additional reference points, though keep in mind that these numbers are guidelines, not rigid targets. Aim for slow, sustainable weight loss of no more than 0.5 to 1 pound per week. Anything faster than that risks muscle loss, reduced milk supply, and metabolic slowdown.
When it comes to exercise, prioritize strength training over cardio for metabolism. Rebuilding and maintaining muscle mass is the most effective long-term strategy for supporting a healthy BMR. Muscle tissue is metabolically active, meaning it burns calories even at rest, so investing in strength now pays dividends for years to come.
Red Flags to Watch For
While some metabolic fluctuation is completely normal during the postpartum period, certain symptoms may signal something more serious. Watch for extreme fatigue that goes beyond normal new-parent tiredness, as this could indicate a thyroid problem or nutrient deficiency. Rapid unexpected weight loss or weight gain that does not match your eating and activity patterns is another warning sign.
Other red flags include significant hair loss, feeling unusually cold all the time, and persistent mood changes beyond typical postpartum adjustment. These could be signs of postpartum thyroiditis, a condition that affects roughly 5 to 10 percent of women after delivery. If you experience any of these symptoms, see your doctor promptly. Early detection and treatment make a significant difference.
What to Do Next
- Talk to your doctor about your specific nutrition needs during pregnancy or postpartum. No article can replace personalized medical guidance.
- Use our BMR calculator as a starting reference point to understand your baseline metabolic rate before or after pregnancy.
- Remember that every pregnancy and recovery is different. Comparing yourself to others or to your pre-pregnancy self is natural but not always helpful. Your body, your timeline, your pace.
- Be patient and kind with yourself during this transition. Growing and delivering a human being is the most physically demanding thing your body will ever do. Give yourself the grace and time you deserve.
Frequently Asked Questions
Does BMR increase during pregnancy?
Yes. BMR gradually increases during pregnancy, rising roughly 5 percent in the first trimester, 10 percent in the second, and up to 20 to 30 percent by the third trimester. This extra energy supports the growing baby, placenta, increased blood volume, and other changes.
How many extra calories do I need while pregnant?
General guidelines suggest no extra calories in the first trimester, about 340 extra per day in the second trimester, and about 450 extra per day in the third trimester. However, individual needs vary significantly so always follow your doctor's advice.
When does metabolism return to normal after birth?
Most women's BMR begins returning to pre-pregnancy levels within a few months postpartum. Breastfeeding keeps metabolism slightly elevated. Full metabolic normalization can take six to twelve months or longer depending on factors like sleep, activity, and hormones.
Does breastfeeding increase BMR?
Yes. Breastfeeding can increase your daily calorie needs by 300 to 500 calories. This is why some women find it easier to lose weight while nursing, though individual experiences vary widely and weight loss should never be the primary goal while breastfeeding.
Should I diet right after having a baby?
Most doctors recommend waiting at least six weeks postpartum before any intentional calorie restriction, and longer if breastfeeding. Focus on nourishing your body with whole foods, staying hydrated, and getting rest. Gradual, gentle approaches are safest for both you and your baby.
Important: This article is for general informational purposes only and is NOT a substitute for professional medical advice. Pregnancy and postpartum nutrition needs are highly individual. Always follow the guidance of your OB-GYN, midwife, or registered dietitian.