Medical disclaimer: This article provides general education and does not diagnose illness. For personal treatment choices, consult a clinician or pharmacist.
A stuffy nose and cough can feel minor at first, then suddenly disrupt sleep, feeding, school, and work. Many families ask the same practical questions: what helps quickly, what is safe for babies, and when should we stop home care and call a doctor? The answer depends on age, symptom pattern, medical history, and warning signs. In general, hydration, saline, humidified air, and rest are foundational. But some medicine choices are age-limited, and breathing symptoms can become urgent. This guide gives a medically careful, family-friendly approach so you can make safer decisions without over-treating or delaying needed care.
Why Stuffiness and Cough Happen Together
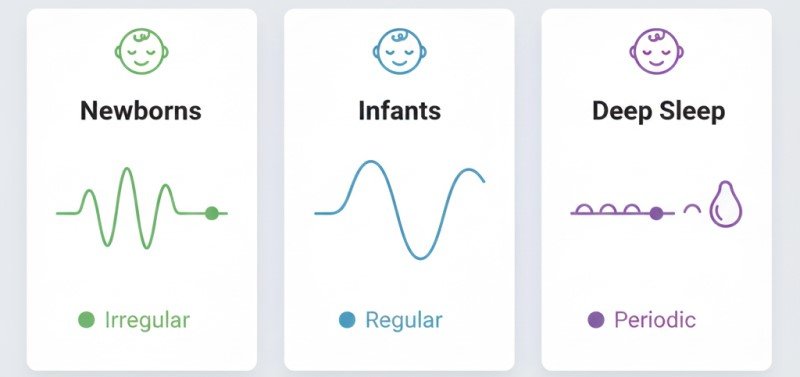
Nasal congestion often increases post-nasal drip, which irritates the throat and triggers cough. Viral infections, allergies, dry air, smoke exposure, and sinus irritation can all produce this pattern. In children, narrow airways and inability to clear mucus can make symptoms seem more dramatic, especially at night.
First-Line Home Care That Is Usually Low Risk
- Hydration: Warm fluids and regular intake help thin secretions.
- Humidified air: Cool-mist humidifier can reduce dryness irritation.
- Saline: Saline drops/sprays or rinses may ease nasal blockage.
- Rest: Sleep and recovery reduce symptom burden.
- Air quality: Avoid smoke, vaping aerosols, and strong fragrances.
For baby-focused guidance, review how to clear baby chest congestion naturally and saline drops for babies guide.
Age-Specific Safety Notes
Babies and toddlers
Do not assume adult OTC products are safe for infants. OTC cough/cold combinations and decongestants may be inappropriate in younger age groups unless a pediatric clinician says otherwise. Focus on hydration, saline, suctioning support, humidity, and clinical assessment when red flags appear.
Older children and adults
Even in adults, decongestants or cough products can have contraindications. If you are pregnant, breastfeeding, have high blood pressure, heart rhythm concerns, thyroid disease, or use other regular medications, confirm safety with a clinician or pharmacist first.
Nighttime Strategy for Better Sleep
- Use saline before bedtime.
- Run a clean cool-mist humidifier overnight.
- Keep room air moderate, not too hot or too dry.
- For babies, follow safe sleep rules and back-sleep guidance.
See best sleeping position for congested baby for child-safe sleep details.
When Symptoms Suggest Flu Instead of a Simple Cold
Flu often starts abruptly with fever, body aches, fatigue, chills, and headache. Congestion and cough may still occur, but systemic symptoms tend to be stronger. If flu is suspected in high-risk people, early medical advice is important. Read flu congestion relief for deeper triage guidance.
Steam vs Nebulizer: Important Safety Distinction
Steam may provide temporary comfort for nasal symptoms in some people but does not deliver asthma medicine. A nebulizer is a medication delivery device when prescribed. Steam should never replace a clinician-directed respiratory treatment plan. For full comparison, read steam inhalation vs nebulizer.
When to See a Doctor
- Symptoms lasting beyond 10 to 14 days without improvement
- Repeated nighttime cough and sleep disruption
- Ear pain, sinus pain, or persistent high fever
- Worsening cough after brief improvement
- Underlying asthma, COPD, or immune vulnerability
Urgent Care Red Flags
- Breathing difficulty, chest retractions, or fast breathing
- Blue lips/face, confusion, faintness, unusual drowsiness
- Dehydration signs (minimal urine, dry mouth, lethargy)
- In infants under 3 months, fever requires prompt assessment
- Severe wheeze or worsening symptoms despite prescribed treatment
If your child has wheeze concerns, see baby wheezing warning signs and when to take baby to doctor for chest congestion.
Medication Education Links
Reminder: these pages are general medication education for adults/general audiences, not instructions for infants.
Symptom Tracking Framework You Can Use at Home
A simple tracking routine helps families decide whether home care is working or whether a clinician review is needed. Check symptoms in the morning and evening: breathing comfort, fever trend, fluid intake, urine output, sleep quality, and energy level. If two or more indicators worsen over 24 hours, escalate care rather than adding multiple new remedies at once.
For children, include feeding tolerance, number of wet diapers, and breathing effort during sleep. For adults, include chest discomfort, activity tolerance, and whether cough is improving or becoming more frequent. This structure reduces guesswork and avoids delayed treatment.
Common Mistakes That Delay Recovery
- Using many OTC products at once without checking duplicate ingredients.
- Ignoring hydration while focusing only on medicines.
- Using strong sprays longer than recommended and triggering rebound congestion.
- Applying adult medicine assumptions to babies or toddlers.
- Waiting too long to seek care when breathing signs worsen.
If your home plan feels increasingly complicated, simplify and call a clinician or pharmacist. A clearer plan is often safer than stacking products.
Practical Day-by-Day Recovery Plan
Day 1-2: prioritize fluids, rest, saline, humidity, and symptom logging.
Day 3-4: assess trend. If improving, continue core care. If worsening, seek clinical review.
Day 5+: unresolved symptoms, recurring fever, or persistent breathing difficulty should be evaluated.
Frequently Asked Questions
Medical disclaimer: FAQ responses are informational and not a prescription.Hydration, saline, humidity, and rest are common first-line options. If symptoms worsen, seek medical review.
No. They may be unsuitable in pregnancy, certain chronic conditions, and younger children.
Do not give OTC cough/cold medicine to babies unless a pediatric clinician advises it.
Breathing distress, dehydration, persistent fever, or worsening illness patterns need urgent assessment.
No. Steam does not replace prescribed respiratory treatment.
Yes, often with systemic symptoms like fever, body aches, and marked fatigue.